Each victim’s encounter with shingles is highly personalized and unique, even though pain, rash, and blisters are the customary trio of complaints. Notice I listed 'pain' first. There’s a reason for that and I don’t think anyone would argue that it ranks number one in attention-getting priority. A friend of mine, who happens to be a nurse, succinctly said, "That’s ouchy." My own descriptive vocabulary has been a tad more salty.
Shingles will in all probability give you some warning that it is about to pounce on you with a fury, but the early warning signals may be difficult to interpret. I’ve heard it described as a burning sensation on the skin, similar to sunburn. What I experienced didn’t feel like that to me. It began with peculiar little sporadic electric jolts of pain over one eyebrow and on my forehead. These areas became quite tender to the touch and I developed a headache. I felt a band of pressure across the right side of my head. Since I am prone to migraines, I promptly began comparing symptoms. This wasn't my typical migraine. The symptoms also refused to respond to my arsenal of OTC (over-the-counter) pain-killers.
Each day that passed the complex pain became more brutal and impossible to ignore; the ‘electric shock treatments’ intensified. The tender areas felt like fresh bruises that hadn’t turned color yet. I brooded over the multiple locations of stabbing pain and compared it with of a couple bouts I’d had with TMJ (temporomandibular joint dysfunction). I was on the right track in the sense that this involved facial nerve pain, yet it wasn’t quite equivalent. Aside from the headache, this pain stayed more localized on the surface, rather than the deep-rooted agony of TMJ. I was so perplexed I honestly didn’t know if I needed a dentist, chiropractor, or physician.
I approached my husband on the morning of the fourth day and announced, “I’m raising the white flag of surrender. I give up. I’m phoning our doctor.” My general practitioner, a hero in my eyes, was completely booked up, so I accepted an appointment with another doctor in the practice. At that point I would have gratefully accepted an encounter with the city dog-catcher as long as he promised to shoot me with a tranquilizer dart.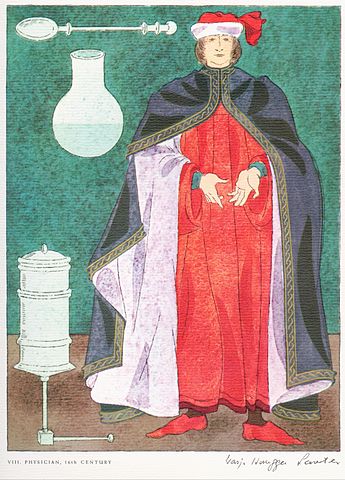
I’m embarrassed to admit it, but I was so worn out from pain and lack of sleep that my emotional state got the better of me. I sat on the paper-covered table in tears, pointing miserably to my head. I tried to explain my personal history with TMJ and migraines and, more importantly, that this wasn’t the same. The unfortunate doctor who got stuck with me was compassionate, but was left trying to judge what to do based on the fact that my head hurt. His diagnoses was that it was an ‘evolving migraine’ and had the nurse give an injection for pain in my derriere (personally, that seemed like the wrong end of the problem, if you follow my drift) and a prescription for a strong pain-reliever to take when I got home. He informed me that he was on-call that night, but if things got really bad I should go straight to the ER. I was instructed to check back in by phone first thing in the morning.
Physician, 16th Century ... portrayed by the Swiss illustrator, Warja Honegger-Lavater, from authentic costume reproductions in the University of Rome's Institute of Medical History. Wikimedia Commons
The pain medication didn’t even touch my symptoms. First thing in the morning I looked in the mirror and saw a slight rash along my eyebrow and up my forehead. It felt like I had tripped and fallen face first into a cactus patch. Realization stuck me just as hard as that first thorny stab of pain five days ago. That unbridled, galloping monster bearing the name ‘shingles’ was leaving its hoof marks right across my face. Back to the doctor’s office I rushed for confirmation.
The good news is that there is an antiviral medication. Although not a cure, it halts the replication of the virus, thereby decreasing the severity and duration of the outbreak. The medicine helps the blisters and sores heal faster, while affecting the development of new ones forming. It may also shorten how long nerve pain lingers after the sores heal. Postherpetic pain can persist for months, or even years. The symptoms can also recur after a long period of latency. Getting the prescription medication as soon as possible, and following directions, is critical to achieving the most positive outcome in your particular situation.
More Articles
- Medicare Advantage Increasingly Popular With Seniors — But Not Hospitals and Doctors
- National Institutes of Health: Common Misconceptions About Vitamins and Minerals
- Julia Sneden Redux: Age Rage; Sometimes You Just Have to Strike Back
- Medical Billing and Collections Among Older Americans
- A Yale Medicine Doctor Explains How Naloxone, a Medication That Reverses an Opioid Overdose, Works
- Kaiser Health News Research Roundup: Pan-Coronavirus Vaccine; Long Covid; Supplemental Vitamin D; Cell Movement
- How They Did It: Tampa Bay Times Reporters Expose High Airborne Lead Levels at Florida Recycling Factory
- Shhhhhh by Ferida Wolff
- Women Consistently Earn Less Than Men; Women Are Over-represented in Lower Paying Jobs and, As They Age, the Pay Gap Widens Even More
- Rose Madeline Mula Writes: I’ve Got A Secret – NOT!






