Update Before Thanksgiving: FDA Investigating Multistate Outbreak of E. coli Infections Likely Linked to Romaine Lettuce and A Warning From the CDC About Raw Turkey Products
Update Before Thanksgiving:
FDA Investigating Multistate Outbreak of E. coli O157:H7 Infections Likely Linked to Romaine Lettuce
The FDA, along with CDC, state and local agencies, is investigating a multistate outbreak of E. coli O157:H7 illnesses likely linked to romaine lettuce. The Public Health Agency of Canada (PHAC) and Canadian Food Inspection Agency, are also coordinating with U.S. agencies as they investigate a similar outbreak in Canada.
Genetic analysis of the E. coli O157:H7 strains tested to date from patients in this current outbreak are similar to strains of E. coli O157:H7 associated with a previous outbreak from the Fall of 2017 that also affected consumers in both Canada and the U.S. The 2017 outbreak of E. coli O157:H7 was associated with leafy greens in the U.S. and romaine in Canada. This year, romaine lettuce is the suspected vehicle for both the U.S. and Canadian outbreaks. There is no genetic link between the current outbreak and the E.coli O157:H7 outbreak linked to romaine that occurred in the Spring of 2018.
The FDA is conducting a traceback investigation to determine the source of the romaine lettuce eaten by people who became sick. Additionally, FDA and states are conducting laboratory analysis of romaine lettuce samples potentially linked to the current outbreak.
The most recent illness onset in the U.S. in the current outbreak was October 31, 2018. For this outbreak investigation, the average interval between when a person becomes ill and when the illness is reported to CDC is 20 days.
Recommendation:
People should not eat romaine lettuce until more is known about the source of the contaminated lettuce and the status of the outbreak.
Outbreak of Multidrug-Resistant Salmonella Infections Linked to Raw Turkey Products
Posted November 8, 2018 at 11:45 AM EDT
CDC and public health and regulatory officials in several states are investigating a multistate outbreak of multidrug-resistant Salmonella infections linked to raw turkey products. The U.S. Department of Agriculture’s Food Safety and Inspection Service (USDA-FSIS) is monitoring the outbreak.
- Reported Cases: 164
- States: 35
- Hospitalizations: 63
- Deaths: 1
- Seventy-four more ill people from 26 states were added to this investigation since the last update on July 19, 2018.
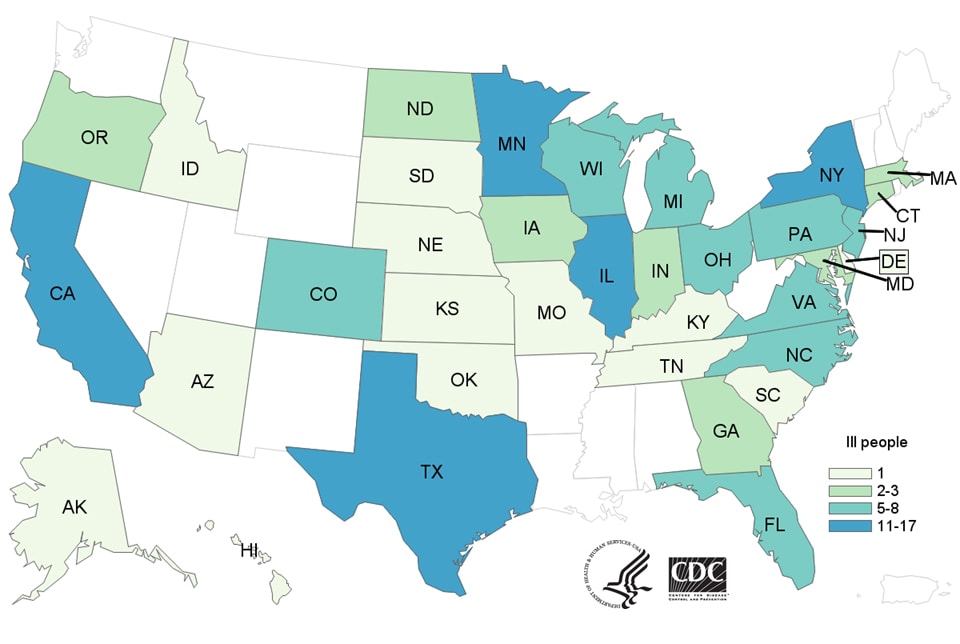
- As of November 5, 2018, 164 people infected with the outbreak strain of Salmonella Reading have been reported from 35 states.
- 63 people have been hospitalized, and one death has been reported from California.
- Epidemiologic and laboratory evidence indicates that raw turkey products from a variety of sources are contaminated with Salmonella Reading and are making people sick.
- In interviews, ill people report eating different types and brands of turkey products purchased from many different locations. Three ill people lived in households where raw turkey pet food was fed to pets.
- The outbreak strain has been identified in samples taken from raw turkey pet food, raw turkey products, and live turkeys.
- A single, common supplier of raw turkey products or of live turkeys has not been identified.
- The outbreak strain of Salmonella Reading is present in live turkeys and in many types of raw turkey products, indicating it might be widespread in the turkey industry. CDC and USDA-FSIS have shared this information with representatives from the turkey industry and asked about steps that they may be taking to reduce Salmonella contamination
Advice to Consumers and Retailers
Always handle raw turkey carefully and cook it thoroughly to prevent food poisoning. This outbreak is a reminder that raw turkey products can have germs that spread around food preparation areas and can make you sick.
CDC is not advising that consumers avoid eating properly cooked turkey products, or that retailers stop selling raw turkey products.
CDC advises consumers to follow these steps to help prevent Salmonella infection from raw turkey:
- Wash your hands. Salmonella infections can spread from one person to another. Wash hands before and after preparing or eating food, after contact with animals, and after using the restroom or changing diapers.
- Cook raw turkey thoroughly to kill harmful germs. Turkey breasts, whole turkeys, and ground poultry, including turkey burgers, casseroles, and sausage, should always be cooked to an internal temperature of 165°F to kill harmful germs. Leftovers should be reheated to 165°F. Use a food thermometer to check, and place it in the thickest part of the food.
- Don’t spread germs from raw turkey around food preparation areas. Washing raw poultry before cooking is not recommended. Germs in raw poultry juices can spread to other areas and foods. Thoroughly wash hands, counters, cutting boards, and utensils with warm, soapy water after they touch raw turkey. Use a separate cutting board for raw turkey and other raw meats if possible.
- Thaw turkey in the refrigerator, in a sink of cold water that is changed every 30 minutes, or in the microwave. Never thaw your turkey by leaving it out on the counter.
- CDC does not recommend feeding raw diets to pets. Germs like Salmonella in raw pet food can make your pets sick. Your family also can get sick by handling the raw food or by taking care of your pet.
CDC will update the advice to consumers and retailers if more information comes available, such as a supplier or type of raw turkey product linked to illness.
- Reported Cases: 164
- States: 35
- Hospitalizations: 63
- Deaths: 1

FDA Plans to Name Stores That Potentially Sold Unsafe Food
By Sandra Eskin of the Pew Charitable Trusts
New U.S. Food and Drug Administration (FDA) draft guidelines better protect consumers from contaminated food by broadening and clarifying circumstances in which the agency will release the names and addresses of stores where recalled products might have been sold.
This is a significant, positive change in FDA’s food safety policies, and one that The Pew Charitable Trusts and 10 other public health groups had urged because store information can help people determine whether they may have bought or eaten potentially dangerous items. Previously, agency officials often said they were required to keep retailer information from the public, even amid outbreaks such as one linked to papayas in 2017 that resulted in more than 230 Salmonella infections.
In the draft guidance, FDA states that it will no longer focus on the confidential nature of the information but, rather, on whether communicating these details can help “effectuate a recall.” To that end, the agency proposes to disclose information about retailers when two conditions are met:
- The product being recalled is not easily identified from its packaging. According to the draft, this could mean foods sold without a universal product code or bar code, or items that lack a lot number or other identifier recognizable to consumers.
- The food is likely to still be in a consumer’s possession based on its shelf life or perishability.
FDA will also consider publicizing retailer information in other situations that do not meet this two-part test, especially when a recalled food is associated with a foodborne illness outbreak.
Finally, the agency suggests that it may release retailer information during recalls of items that pose lower risks to public health but are difficult for people to identify because the items lack or have minimal packaging. Fruits, vegetables, and products sold in bulk such as nuts are among the examples FDA gave in its guidelines.
Consumers should keep in mind that the agency’s store lists won’t necessarily be comprehensive or completely accurate. Moreover, retailers not named in FDA’s announcements could carry food covered by a recall. The nation’s vast and frequently complex food supply chain makes it challenging for FDA to collect and verify information about all locations where a product may be sold. And though companies involved in the recall may be able to provide additional details, they, too, face obstacles in tracing food products from the farm or manufacturer to the point of sale.
Despite these limitations, FDA’s expanded guidelines are unquestionably a big victory for consumers and public health. The new policy brings a more consistent and transparent approach to announcements essential to helping Americans protect themselves and their families from foodborne diseases. And it closely aligns how the FDA — which oversees about 80 percent of the food supply — communicates about recalls with comparable practices at the U.S. Department of Agriculture, where meat and poultry products are regulated. That’s progress worth celebrating.
Sandra Eskin directs The Pew Charitable Trusts’ work on food safety.
More Articles
- Encore: Kitchen Stigmata and There Are Many Ways to Identify a Good Cook by Julia Sneden
- Department of Labor Awards $5M to Train, Expand Pathways for Women for Registered Apprenticeships, Nontraditional Occupations
- Monetary Policy Report Prepared at the Federal Reserve Bank of Richmond, Expectations for Future Growth Were Mostly Unchanged
- A Yale Medicine Doctor Explains How Naloxone, a Medication That Reverses an Opioid Overdose, Works
- Center for Strategic and International Studies: “The Future Outlook with Dr. Anthony Fauci”
- A Reminder From the White House: Prepare for New Variants As We Work to Keep Ourselves Protected Against COVID-19
- Indoor and Vertical Farming May Be Part of the Solution to Rising Demands for Food and Limited Natural Resources
- Federal Reserve Issues FOMC Statement Signaling a March Interest Rate Hike as Well As Reducing the Size of the Fed's Balance Sheet
- The Federal Open Market Committee Statement: The Path of the Economy Continues to Depend On The Course Of The Virus
- Voting Rights: Assistant Attorney General Kristen Clarke Testifies Before the Senate Judiciary Committee Hearing; “One of the most monumental laws in the entire history of American freedom”






